Abstract
Introduction and background:
Acute myeloid leukemia (AML) is a rare disease that critically disrupts the function of the bone marrow. Genetic mutations and cytogenetic changes are the main culprits of this process. As the bone marrow fails to perform its usual activity, blood production is crucially affected. Patients with AML need immediate access to medical facilities to treat such an acute disease. It has been postulated that a black population may have worse outcomes in AML. The less favorable outcome may result from miscellaneous factors, with social-economical disparities being the most important. In light of the systemic racism in health care and society in general, minorities may have less access to prime health care centers. Many studies suggest racial differences in survival among whites and black populations. But few have compared outcomes based on the ELN genetic risk stratification. It's important to realize that uneven outcomes may also result from more adverse genetic profiles in specific subgroups. In our study, we analyzed the results of the treatment of AML in a single American institution separated by race and ELN risk.
Material and Methods:
In this study, we retrospectively evaluated the outcomes of all patients with AML at our institution. We collected the data from patients treated with AML from June 2020 to June 2022. The most relevant information collected were: self-declared race, age, blood counts, cytogenetics, Next Generation Sequence information, Charlson Comorbidity Index(CCI), type of treatment, the best response to therapy, time to progression, and overall survival. We evaluated a total of 39 patients. Seventeen individuals were classified as adverse risk and twenty-two as an intermediate or good risk. Overall survival and statistical analysis were performed in all patients, and a special subanalysis was also done in the adverse risk group. Twenty-two patients self-declared as whites and 17 as black.
Results:
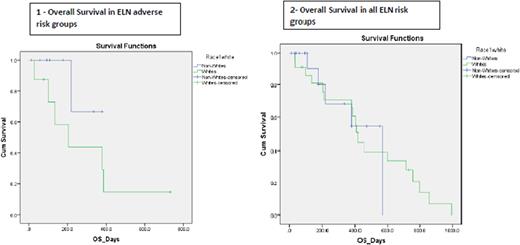
Among all ELN risk groups(figure 2), the estimated mean time until death was 417.21 days for blacks and 476.81 days for whites. At 400 days, the probability of survival was approximately 0.40 (or 40%) for blacks and 0.55 (or 55%) for whites. As the p-value (0.996) was greater than 0.05, we concluded that there was insignificant evidence of a difference in survival times for whites and blacks in all ELN risk groups. In a subanalysis of the ELN adverse risk population(figure 1), the estimated mean time until death was 326.00 days for non-whites and 285.96 days for whites. At 200 days, the probability of survival was approximately 0.68 (or 68%) for blacks and 0.43 (or 43%) for whites. As the p-value (0.187) was greater than 0.05, we again concluded that there was insignificant evidence of a difference in survival times for whites and blacks, even in adverse risk ELN subgroups.
Conclusions and recommendations:
Our study has identified no statistical difference in survival between whites and blacks in our single university institution population. Moreover, the evaluation in the adverse risk patients showed that at 200 days, the probability of survival in blacks is numerically higher than in whites. These results contradict the idea that a white population tends to have better outcomes than a black population regarding AML. The study's obvious limitation is the small sample population and the short follow-up period. Given equal access to care, as in our institution, outcomes were similar regardless of race. Further studies should be performed to evaluate the differences in outcomes among black and whites to validate our findings.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.